
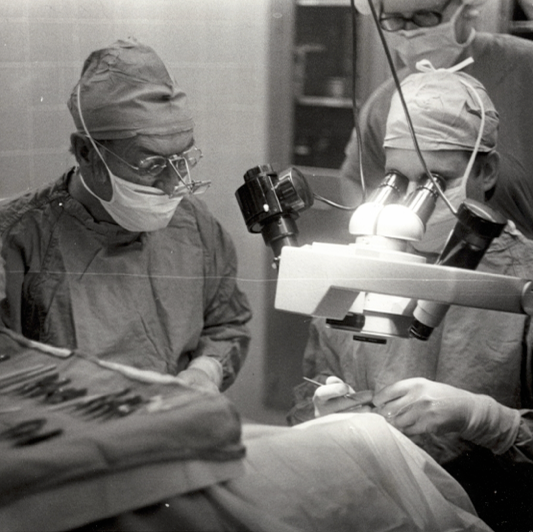
50 YEARS OF BEING "FOR SURGEONS"
Since 1974, ASCRS has supported surgeons through some trying times and has championed their triumphs. With the backing of its members and its innovative spirit throughout these past 50 years ASCRS has advanced the education, advocacy, and philanthropy of anterior segment surgery.
Learn more about the historyEssential tools for your practice
2024 Annual Meeting Post-Meeting Resources
Claim Credit for the 2024 ASCRS Annual Meeting
We value your feedback!Complete the 2024 ASCRS Annual Meeting Evaluation and Credit Claim online by April 29, 2024. You will need your Badge ID to log into the evaluation site.
2024 ASCRS Annual Meeting On Demand
The ASCRS Annual Meeting On Demand provides physician meeting registrants with unprecedented digital access to the 2024 ASCRS Annual Meeting in Boston, MA. Access the 2024 ASCRS On Demand content at your convenience and catch all the sessions you missed in Boston.
Find Your Place Here
ASCRS, the largest U.S. membership society dedicated to meeting the needs of anterior segment surgeons at every career stage, offers a range of member benefits. Explore these exclusive benefits!ASCRS Live! Dinner Series
ASCRS Live! is a new regional dinner series coming to nine cities in 2024. The primary focus at each event will be refractive cataract surgery along with a secondary, rotating topic. These events, open to local members and nonmembers, will include ample time for open discussion and questions.
Learn More

Exceptional Education in ASCRS CME 24/7
Your source for the latest online CME
ASCRS CME 24/7 is your resource for online CME activities, providing high quality CME education at your convenience. Explore the variety of CME available to meet your clinical area of interest, including:
A Taste of ASCRS—A program designed to offer a "taste" of the best education ASCRS has to offer
ASCRS Grand Rounds—The experience of a grand rounds in your home or office
ASCRS Satellite CME—a series of online CME activities focused on the latest techniques and technologies




