2022 MEDICARE PHYSICIAN FEE SCHEDULE (MPFS)
FINAL RULE RELEASED
CMS Accepts RUC Recommended Values for New Cataract/MIGS Combination Codes; ASCRS, AAO, and AGS Advocacy Results in Increase from Original CMS Proposal
No Changes to Mitigate the Pending Payment Cuts Associated with the 2021 Increases to the Standalone E/M Codes
Includes 2022 Quality Payment Program Changes
2022 Conversion Factor: $33.5983
This afternoon, CMS released the CY 2022 MPFS Final Rule. CMS also released a press release, a physician fee schedule fact sheet, and a QPP fact sheet.
2022 MPFS Conversion Factor
The CY 2022 MPFS conversion factor is $33.5983, a decrease of approximately 3.78% ($1.30) from the CY 2021 MPFS conversion factor of $34.8931. The CY 2022 final MPFS conversion factor reflects a budget neutrality adjustment of -0.10%, the expiration of the 3.75% payment increase provided for CY 2021 by the Consolidated Appropriations Act, and the 0.00% update adjustment factor as established in MACRA.
According to the CMS estimated impact on total allowed charges by specialty, ophthalmology is impacted by 0%. For CY 2022, the Medicare payment rate for 66984 is $528.84, a decrease of $19.33 from the CY 2021 Medicare payment of $548.17.
We will continue to advocate with the medical and surgical community, urging Congress to prevent these Medicare physician payment cuts from taking effect.
CMS Accepts AMA RUC Recommended Values for New Cataract and Microinvasive Glaucoma Surgery (MIGS) Combination Codes
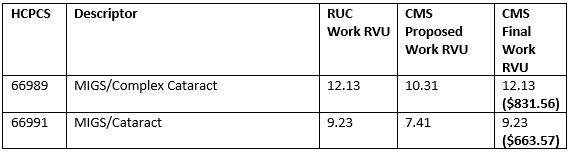
As a result of ASCRS, AAO, and AGS advocacy, CMS has accepted the AMA RUC recommended values, which result in an increase in their originally proposed work RVUs for the new Category I CPT codes that describe MIGS procedures when performed in conjunction with cataract surgery in its final rule. As a reminder, in the 2022 MPFS proposed rule, CMS recommended outrageously low work values for CPT 66989 (10.31 WRVU) and 66991 (7.41 WRVU). This was solely based on time and failed to recognize the necessary incremental work in addition to the corresponding standalone cataract intraocular lens procedures. Additionally, the proposed values would have destroyed the relativity between the cataract family of procedures.
The table below shows the RUC work RVU recommendations, the CMS proposed work RVU, and the finalized recommendation.
Additionally, CMS encourages the RUC to reconsider the valuation of the cataract procedure family as a whole, including the new codes, in the near term.
E/M Visits
CMS is refining its longstanding policies for split (or shared) E/M visits to reflect the role of non-physician practitioners (NPPs) as members of the medical team, and to clarify conditions of payment that must be met to bill Medicare for these services. In the CY 2022 MPFS final rule, CMS is establishing the following:
- Definition of split (or shared) E/M visits as E/M visits provided in the facility setting by a physician and an NPP in the same group. The visit is billed by the physician or practitioner who provides the substantive portion of the visit.
- By 2023, the substantive portion of the visit will be defined as more than half of the total time spent. For 2022, the substantive portion can be history, physical exam, medical decision-making, or more than half of the total time (except for critical care, which can only be more than half of the total time).
- Split (or shared) visits can be reported for new as well as established patients, and initial and subsequent visits, as well as prolonged services.
- A modifier is required on the claim to identify these services to inform policy and help ensure program integrity.
- Documentation in the medical record must identify the two individuals who performed the visit. The individual providing the substantive portion must sign and date the medical record.
- Codifying these revised policies in a new regulation at 42 CFR 415.140.
E/M Post-operative Visits in the 10- and 90- day Global Surgical Codes
Unfortunately, this final rule does not include increases to the value of E/M post-operative services in 10- and 90-day global surgery codes. ASCRS will continue to work with the surgical community advocating that Congress direct the CMS to adjust the values of the E/M post-operative visits included in 10-day and 90-day global surgical codes to reflect the updated office/outpatient E/M code payment increases that were implemented on January 1, 2021.
Medicare Telehealth Services
- For CY 2022, CMS finalized that certain services added to the Medicare telehealth services list will remain on the list through December 31, 2023, allowing additional time for the agency to evaluate whether the services should be permanently added to the Medicare telehealth services list. Additionally, CMS is adopting coding and payment for a longer virtual check-in service on a permanent basis.
- The Consolidated Appropriations Act removed the geographic restrictions and added the home of the beneficiary as a permissible originating site for telehealth services furnished for the purposes of diagnosis, evaluation, or treatment of a mental health disorder. It also requires for these services that there must be an in-person, non-telehealth service with the physician or practitioner within six months prior to the initial telehealth service and requires the secretary to establish a frequency for subsequent in-person visits. Therefore, CMS is implementing these statutory amendments, and finalizing that an in-person, non-telehealth visit must be furnished at least every 12 months for these services, that exceptions to the in-person visit requirement may be made based on beneficiary circumstances (with the reason documented in the patient’s medical record), and that more frequent visits are also allowed under our policy, as driven by clinical needs on a case-by-case basis.
Quality Payment Program
MIPS Value Pathways (MVPs)
CMS has developed and finalized 7 new MVPs that will be available beginning with the 2023 performance year, which does not include ophthalmology, as a result of concerns raised by ASCRS and the ophthalmic community. The addition of MVPs is part of a greater effort of CMS to sunset traditional MIPS after the end of the 2027 performance period/2029 payment year. CMS did not finalize the timeframe in which MVP reporting would no longer be voluntary and said any proposal to sunset traditional MIPS will be made in future rulemaking.
Performance Threshold Proposals
CMS established the performance threshold using the mean final score from the 2017 performance year/2019 MIPS payment year, which will result in a performance threshold of 75 points. The additional performance threshold will be 89 points. The additional MIPS adjustment factors for exceptional performance are available through the 2022 performance year/2024 MIPS payment year, making this the last year of the additional performance threshold and the associated additional MIPS adjustment factors for exceptional performance.
Performance Category Weights
For the 2022 performance year/2024 payment year, CMS finalized the following performance category weights:
- 30% for the Quality performance category.
- 30% for the Cost performance category.
- 15% for the Improvement Activities performance category.
- 25% for the Promoting Interoperability performance category.
Additional Details to Come
Additional information will be detailed in upcoming editions of Washington Watch Weekly.



